Costochondral pain after strenuous endurance exercise. Rojas-Valverde D. y col. ISSN 2215-5562. Rev. Ter. Enero-Junio de 2022; Vol. 16 N°1: 96-103.
REPORTE DE CASO
Orthopedic manipulative therapeutic approach of costochondral pain after combined strenuous endurance exercise: a case report
Abordaje por terapia manual ortopédica del dolor costo-condral posterior a una combinación de ejercicios de resistencia extenuantes: un reporte de caso
Título corto: Approach of costochondral pain after strenuous endurance exercise
Autores: Daniel Rojas-Valverde1,2, Diego Ruiz-Yanarella3
Filiación: 1Centro de Investigación y Diagnóstico en Salud y Deporte (CIDISAD), Escuela Ciencias del Movimiento Humano y Calidad de Vida (CIEMHCAVI), Universidad Nacional, Heredia, Costa Rica. 2Clínica de Lesiones Deportivas (Rehab & Readapt), Escuela Ciencias del Movimiento Humano y Calidad de Vida (CIEMHCAVI), Universidad Nacional, Heredia, Costa Rica. 3Escuela de Terapia Física, Universidad Santa Paula, San José, Costa Rica.
Autor de correspondencia: Daniel Rojas-Valverde, email: drojasv@una.cr
Forma de citar: Rojas-Valverde D, Ruiz-Yanarella D. Orthopedic manipulative therapeutic approach of costochondral pain after combined strenuous endurance exercise: a case report. Rev Ter. 2022;16(1): 96-103.
Financiamiento: ninguno.
Fecha de envío: 1 de agosto del 2021.
Fecha de aceptación: 27 de diciembre del 2021.
Conflictos de interés: ninguno.
Abreviaturas: POLD, pulsation oscillation long duration.
Abstract
The purpose of this case study was to present the effectiveness of physiotherapeutic treatment based on manual orthopedic techniques in an amateur athlete with costochondritis due to physical strenuous exercise. A 31 years old experienced, well-trained, endurance amateur athlete presented chest pain suggesting costochondritis after physical and kinetic examination. Patient reported to present pain after physical effort in the last two weeks (combination of mountain biking, route cycling, running, swimming and yoga). Manual therapy including techniques as resonant oscillation mobilization of the thoracic region, Lewit´s post-isometric relaxation and sliding of the right humeral head, cervico-thoracic high speed technique mobilization, active-assisted mobilization of 7th to 10th ribs during expiratory phase, superficial myofascial induction in lower costal area and, muscle power technique, is effective to relieve pain increase mobility of cervical rotation, increase mobility of glenohumeral joint (e.g., internal rotation), in an amateur athlete with costochondritis due to physical strenuous exercise.
Keywords: chest pain, manual therapy, physical endurance, acute injury.
Resumen
El propósito de este caso de estudio fue presentar la efectividad del tratamiento fisioterapéutico basado en técnicas ortopédicas manuales en un deportista aficionado con costocondritis por ejercicio físico intenso. Un deportista aficionado de resistencia de 31 años, experimentado, bien entrenado, que presentó dolor torácico sugestivo de costocondritis después de un examen físico y cinético. El paciente refirió presentar dolor después del esfuerzo físico en las últimas dos semanas (combinación de bicicleta de montaña, ciclismo de ruta, carrera, natación y yoga). La terapia manual que incluye técnicas como movilización por oscilación resonante de la región torácica, relajación post-isométrica de Lewit y deslizamiento de la cabeza humeral derecha, movilización con técnica de alta velocidad cervico-torácica, movilización activa asistida de la séptima a la décima costilla durante la fase espiratoria, inducción miofascial superficial en la zona costal inferior y, la técnica de potencia muscular, es eficaz para aliviar el dolor aumentar la movilidad de la rotación cervical, aumentar la movilidad de la articulación glenohumeral (p. ej., rotación interna), en un atleta aficionado con costocondritis debido al ejercicio físico extenuante.
Palabras clave: dolor torácico, terapia manual, resistencia física, lesión aguda.
Introduction
Chest pain can suggest, low, mild and high risk for athletes depending of the contextual, situational conditions of the development of pain, but also depending of the physiopathology. The pain may originate from thorax, usually suggesting issues with structures as heart, lungs, or esophagus. In athletes, musculoskeletal etiology of the chest pain must be considered for diagnose. In this sense musculoskeletal-related chest pain can occur in the ribs, sternum, articulations or myofascial structures1.
The costochondritis, should be differentiated from Tietze’s syndrome, slipping rib syndrome (e.g., clicking rib syndrome) and painful xiphoid syndrome1. It prevalence usually increase if female, Hispanic and Afro-Caribbean and lower socio-economic class2. Additionally, athletes are usually subjected to large indirect forces or overuse caused by physical activity. The most exposed sports are golf, rowing, swimming, baseball, weightlifting, waterskiing or wrestling causing pain and tenderness of the sternum1,3,4.
Costochondritis is presented in a wide variety of signs and symptoms as chest pain, usually at the level of the 2nd to 6th ribs near sternum (costochondral joints)5,6, confined pain that can radiate to a wider area, pressure over the affected area could lead to sharp or aching pain1. A prevalence of 30% of patient reported chest pain are diagnoses with costochondritis, no specific data is available for athletes2. It could be caused by chest or pulmonary infections, large physical efforts as strength and repeated bouts, accidents hitting the chest (trauma) and some types of arthritis. Prognosis is generally good, considering most of cases are mild and settle reasonably quickly and relapse is unlikely.
While the performance of repetitive movement could strain the chest wall, costochondritis could be provoked by endurance exercise like swimming, mountain biking, running, among other activities. The treatment for costochondritis commonly included corticosteroid injection, but alternative physical therapy approaches as manual orthopedic methods are recently used, besides, physical specific exercise is recommended3. Indeed, it is well-known as an effective technique to provoke some benefits for athletes with functional asymmetries7.
Considering that costochondritis is relative uncommon among endurance athletes, the purpose of this case study was to present the effectiveness of physiotherapeutic treatment based on manual orthopedic techniques in an amateur athlete with costochondritis due to physical strenuous exercise. Costochondritis is relative uncommon in primary care, but is not usually referred to physical therapy8. This is why, this article is of special value in demonstrating the efficacy and efficiency of manual therapy as an alternative method to medical treatment (e.g, steroid injections, anti-inflammatory drugs)9.
Clinical Case Report
The patient's information was confidentially accessed, and the authors obtain his consent for the academic, anonymous and confidential publication of her medical record, diagnosis and treatment. This study followed the ethical guidelines in accordance with the Declaration of Helsinki on biomedical research in human beings (18th Medical Assembly, 1964, revised in Fortaleza 2013). All data was collected based on self-report and therapeutic record review. All examination, evaluation and treatment were conducted by an experienced physical therapist with more than ten years of clinical experience and more than five years of orthopedic medic physical therapy training.
Anamnesis
A 31-year-old man arrived to physical therapy clinic with moderate pain in the middle chest (see figure 1). He reported that the pain had persisted progressively since the last two days. He had no history of previous chest pain, fractures, surgery, or trauma. No radicular or referred symptoms were reported.
Patient report to perform a series of endurance activities, mainly triathlon. No history of injuries, acute or chronic diseases neither other exercise related issues nor previous illness. At the moment of the consultation his rest heart rate was 54 bpm. Patient did not intake any drugs or medication. Among other respiratory conditions, patient reported to suffered from COVID-19 three months before consultation. Also, he reported to be partially vaccinated for SARS-CoV-2 (Astra Zeneca).
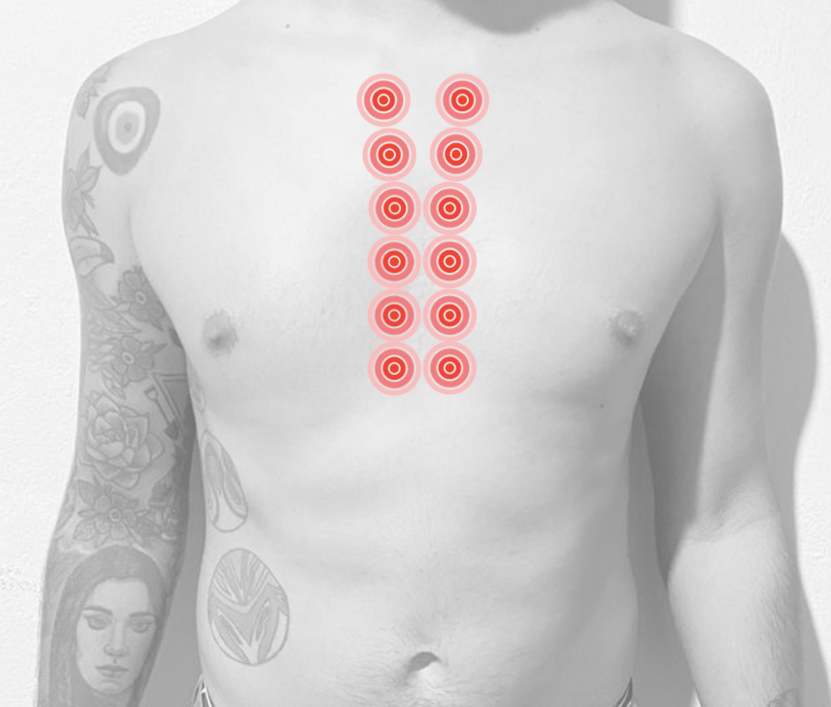
Figure 1. Self-reported area of moderate pain.
Photograph with the consent of the patient
Physical exercise monitoring
Patient had an endurance exercise history of 15 years and was considered as performance level 4 athlete10. Patient report to performed route cycling (30.8km; elevation gain 380m), mountain biking (277.6km, elevation gain 5095m), swimming (500m), yoga (20min) and running (10km, 4:48 pace) sessions the two previous weeks before the physical therapy consultation. He reported to be at the tapering phase for a marathon, to pe performed two days after consultation.
His total sleep was 9h:4min, with average of 13 breaths per min the previous night of the consultation and an average of 8h:29min, with average of 12.7 breaths per min the previous two weeks. Previous the attention the patient had 57 beats per min of rest heart rate and an average of 53.7 beats per min the last two week before consultation.
Kinetic evaluation and findings
The chest pain was assessed using previously stablished key points as onset, location, character, duration, precipitating factor, aggravating factor, relieving factor11. Costochondral pain referred during expiration, anteroposterior chest compression, and cervical and thoracic flexion between 2nd and 5th bilateral costochondral joints. Pain did not increase with active movement of upper limbs or exercise and relieved during rest.
During physical exploration an asymmetry in inclination of the C2 vertebrae was found. The asymmetry was associated to a loss of cranio-vertebral centric relationship, with a deficit in the right subcraneal inclination. Due to an inverse coupling, during cervical left rotation, C1 and C2 rotation was partially compromised.
Besides, some musculoskeletal issues were found as hypertonia of the right pectoralis minor muscle, slight limitation of internal rotation of the left glenohumeral joint, moderate limitation of the internal rotation of the right glenohumeral joint, anteriorization of the right humeral head identified by the assessment of the glenohumeral internal rotation from the 90° abduction, hypomobility of the cervico-thoracic hinge, and lower ribs in elevation and hypertonia of the external oblique muscle.
The costochondritis was differentiated from Tietze syndrome considering previous literature based on the absence of signs of inflammation and swelling, the onset of pain was by repetitive activity, the aggravation of pain was boosted by deep exhalation and breathing, exertional activities and more than 90% of cases is multiple and unilateral, usually with 2nd to 5th costochondral junctions involved3.
Clinical Rationale
Pain in the expiratory phase that did not increased during physical exercise could be influenced by a high cervical condition, which, based on reference frames such as clinical neuro dynamics, potential neural edema that usually generates greater symptoms (eg. Mechanosensitivity during rest), glenohumeral dynamics according to an advanced position of the humeral head that favors the scapular anterior tilt and a facilitation of the kyphotic curve and the consequent irritation of the costovertebral (posterior) joints as well as costo-chondral and chondrosternal (posterior), would be a chain of events that could form an integrated hypothesis that could explain the symptoms in the sternal region.
Although it is not a definitive reasoning, it is a pathway built on the basis of the findings found in the evaluation and in comparison with the other cases of anterior chest pain in which posterior or posterolateral pain predominates and which are generally exacerbated with the inspiratory phase of respiration. Also, hand by hand with the toxic and glenohumeral asymmetries and findings, the great physical exercise bouts the previous two weeks prior consultations could be a factor that exacerbates symptoms.
Therapeutic approach
The therapeutic approach was performed based on manual orthopedic techniques. The therapy consisted in:
1. Superficial myofascial induction in the lower costal region (external oblique and diaphragm)
2. Active-assisted lower-medial mobilization of ribs 7 to 10 during the expiratory phase
3. Axis Low Speed Handling (Right Tilt) (Rocabado´s Approach)
4. Post-isometric relaxation of the suboccipital muscles
5. Postero-lateral sliding of the right humeral head and post isometric relaxation
6. High speed technique mobilization of the cervico-thoracic hinge in prone (bilateral)
7. Pulsation Oscillation Long Duration (POLD) method: resonant oscillation mobilization of the thoracic region in the prone position
8. Teaching exercises to activate and increase recruitment of infraspinatus muscle with garter and muscle power technique
Therapeutic outcomes
After treatment, the relative position of the skull on the upper cervical spine is favored, positively modifying the subcranial lateral inclination capacity in both directions (its effectiveness should be to check with the user in the prone position with head rotation to the left, comparable sign).
There was a spontaneous normalization of the glenohumeral internal rotation of the left shoulder posterior to the superior cervical approach. The improvement hypothesis was based on the reduction of mechanical stress of the contact surface on the brachial plexus and its terminal branches at shoulder level.
The internal rotation of the right shoulder did not show a change in range of motion as well as in the end-feel, for which a true dysfunction was evidenced at the joint level in which the neurodynamic and high cervical factor had no significant influence.
All mobilization and myofascial approaches aimed to improve thoracic dynamics due to the absence of direct techniques at the sternal level in this therapeutic modality. Also functional asymmetries were treated as factors boosting the costochondral pain.
Discussion
The aim of the present study was to present the effectiveness of physiotherapeutic treatment based on manual orthopedic techniques in an amateur athlete with costochondritis due to physical strenuous exercise. The manual therapy approach was effective to relieve pain, increase mobility of cervical rotation, increase mobility of glenohumeral joint (e.g., internal rotation).
While major of the causes for costochondritis were discarded due to the clinical history and anamnesis, physical effort and strenuous repetitive exercise was considered the cause of the chest pain3,9. In this sense, most of the pain related to muscles are provoked by muscle strains as pectoralis muscle strains, injuries to internal and external obliques muscles, serratus anterior muscle injury3. This is why the manual therapy have been proposed as an useful method to chest pain relieve (e.g., costochondritis)12,13.
When patients are referred to physical therapy, often the costochondritis had progressed to a chronic stage with endurance and strength impairments. This is why it is essential to refer these cases to physical therapy and physical training professionals for manual therapy, pain relieve approaches and exercise prescription. The infrequent referral of patient with costochondritis to physical therapy services has made it difficult for reporting, controlling and systematizing this kind of cases and the efficacy and efficiency of therapeutic approach to this acute issue. Additionally, there is a lack of consensus regarding the treatment strategies for costochondritis in general populations and especially athletes8.
It has been studied that diaphragmatic stretching and myofascial induction improved cervical and lumbar mobility and increased ribcage movement at xyphoid level14, potentially improving pain during breathing in costochondritis. Costochondritis and related pain could limit the range of movement and affect muscle properties (e.g., external and internal oblique, diaphragm), this is why it is essential to explore muscle chains and potential compensation in adjacent and also relative distant muscles15. Therefore, diaphragm as primary muscle of respiration, involved in postural stability and control, should be evaluated and treated as in the present case.
Besides, the treatment of cervical and shoulder joints and muscles is essential in chest issues due to the essential role of these structures in breathing (e.g, scalenus, sternocleidomastoid, pectoralis minor, clavicular, upper trapezius, dorsal longus). This is why, assessing, handling and recovering through manual therapy the cervical symmetry, craniocervical posture and cervio-toraxic alignment is essential16,17. In this case, Rocabado method16,18 and Lewit´s relaxation and sliding16,19-21 were efficient to recover cervical range of motion and cervical stability and functionality. Finally, the POLD methods was also used due to its properties in joints pain and mobility22. This therapy had shown it efficacy as an better option for the improvement of motion compared to conventional treatment23 .
Conclusion
Manual therapy including techniques as resonant oscillation mobilization of the thoracic region, Lewit´s post-isometric relaxation and sliding of the right humeral head, cervico-thoracic high speed technique mobilization, active-assisted mobilization of 7th to 10th ribs during expiratory phase, superficial myofascial induction in lower costal area and, muscle power technique, is effective to relieve pain increase mobility of cervical rotation, increase mobility of glenohumeral joint (e.g., internal rotation), in an amateur athlete with costochondritis due to physical strenuous exercise
References
- Gregory PL, Biswas AC, Batt ME. Musculoskeletal Problems of the Chest Wall in Athletes. Sports Med. 2002;32(4):235-50. doi: 10.2165/00007256-200232040-00003.
- Disla E, Rhim HR, Reddy A, Karten I, Taranta A. Costochondritis: A Prospective Analysis in an Emergency Department Setting. Arch Intern Med. 1994;154(21):2466-9. doi: 10.1001/archinte.154.21.2466
- Ayloo A, Cvengros T, Marella S. Evaluation and Treatment of Musculoskeletal Chest Pain. Prim Care. 2013;40(4):863-87, viii. doi: 10.1016/j.pop.2013.08.007.
- Hopper MA, Tirman P, Robinson P. Muscle injury of the chest wall and upper extremity. Semin Musculoskelet Radiol. 2010;14(2):122-30. doi: 10.1055/s-0030-1253156.
- Malghem J, Vande Berg BC, Lecouvet FE, Maldague BE. Costal Cartilage Fractures as Revealed on CT and Sonography. AJR Am J Roentgenol. 2001;176(2):429-32. doi: 10.2214/ajr.176.2.1760429.
- Hannan MT, Anderson JJ, Pincus T, Felson DT. Educational attainment and osteoarthritis: Differential associations with radiographic changes and symptom reporting. J Clin Epidemiol. 1992;45(2):139-47. doi: 10.1016/0895-4356(92)90006-9.
- Rojas-Valverde D, Sánchez-García A, Sáenz-Ulloa D, Gutiérrez-Vargas R. Does Osteopathic Manipulation Lead to Improvements in Physical and Muscle Mechanical Function and Spinal Symmetries in Golfers? Kronos [Internet]. 2019;18(1):1-10. Disponible en: https://www.academia.edu/download/64853181/Kronos_Golf.pdf
- Zaruba RA, Wilson E. Impairment based examination and treatment of costochondritis: a case series. Int J Sports Phys Ther [Internet]. 2017;12(3):458-67. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5455195/pdf/ijspt-12-458.pdf
- Proulx AM, Zryd TW. Costochondritis: diagnosis and treatment. Am Fam Physician [Internet]. 2009;80(6):617-20. Disponible en: https://www.aafp.org/afp/2009/0915/afp20090915p617.pdf
- De Pauw K, Roelands B, Cheung SS, de Geus B, Rietjens G, Meeusen R. Guidelines to classify subject groups in sport-science research. Int J Sports Physiol Perform. 2013;8(2):111-22. doi: 10.1123/ijspp.8.2.111.
- Fam AG, Smythe HA. Musculoskeletal chest wall pain. CMAJ [Internet]. 1985;133(5):379-89. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1346531/pdf/canmedaj00268-0035.pdf
- Ian Rabey M. Costochondritis: Are the symptoms and signs due to neurogenic inflammation. Two cases that responded to manual therapy directed towards posterior spinal structures. Man Ther. 2008;13(1):82-6. doi: 10.1016/j.math.2006.12.007.
- Rovetta G, Sessarego P, Monteforte P. Stretching exercises for costochondritis pain. G Ital Med Lav Ergon [Internet]. 2009;31(2):169-71. Disponible en: https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.533.2506&rep=rep1&type=pdf
- González-Álvarez FJ, Valenza MC, Torres-Sánchez I, Cabrera-Martos I, Rodríguez-Torres J, Castellote-Caballero Y. Effects of diaphragm stretching on posterior chain muscle kinematics and rib cage and abdominal excursion: a randomized controlled trial. Braz J Phys Ther. 2016;20(5):405-411. doi: 10.1590/bjpt-rbf.2014.0169.
- Hamaoui A, Le Bozec S, Poupard L, Bouisset S. Does postural chain muscular stiffness reduce postural steadiness in a sitting posture? Gait Posture. 2007;25(2):199-204. doi: 10.1016/j.gaitpost.2006.03.012.
- Sandoval C, Díaz A, Manríquez G. Relationship between craniocervical posture and skeletal class: A statistical multivariate approach for studying Class II and Class III malocclusions. 2021;39(2):133-140. doi: 10.1080/08869634.2019.1603795
- de Oliveira LB, Cajaíba F, Costa W, Rocabado M, Lazo-Osório R, Ribeiro S. Comparative analysis of assessment of the craniocervical equilibrium through two methods: cephalometry of Rocabado and cervical range of motion. 2012;41 Suppl 1:2563-8. doi: 10.3233/WOR-2012-0499-2563.
- Rocabado M. The importance of soft tissue mechanics in stability and instability of the cervical spine: a functional diagnosis for treatment planning. 1987;5(2):130-8. doi: 10.1080/08869634.1987.11678183.
- Czaprowski D, Leszczewska J, Kolwicz A, Pawłowska P, Kędra A, Kriščiūnas A, et al. The Influence of Self-Stretching Based on Postisometrical Relaxation, Static Stretching Combined with Stabilizing Exercises, and Stabilizing Exercises Only on the Flexibility of One-Joint and Two-Joint Hip Flexors. Medicina (Kaunas). 2013;49(10):439-46. doi: 10.3390/medicina49100069
- Emary P. Use of post-isometric relaxation in the chiropractic management of a 55-year-old man with cervical radiculopathy. J Can Chiropr Assoc [Internet]. 2012;56(1):9-17. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3280114/pdf/jcca-v56-1-009.pdf
- Liebenson C. Self-treatment of mid-thoracic dysfunction: a key link in the body axis: Part Two: Treatment. J Bod Mov Ther. 2001;5(3):191-5. doi: 10.1054/jbmt.2000.0226
- Pavón E. Eficacia del método POLD en el tratamiento de trastornos cervicales [Tesis de Licenciatura en Kinesiología]. Buenos Aires: Universidad FASTA; 2015. Disponible en: http://redi.ufasta.edu.ar:8080/xmlui/handle/123456789/810
- López-Díaz JV, Arias-Buría JL, Lopez-Gordo E, Lopez Gordo S, Aros Oyarzún AP. “Effectiveness of continuous vertebral resonant oscillation using the POLD method in the treatment of lumbar disc hernia”. A randomized controlled pilot study. Man Ther. 2015;20(3):481-6. doi: 10.1016/j.math.2014.11.013.